Colorado senators review budget as Medicaid costs drive $776 million increase

Colorado senators this week are reviewing revisions to the current state budget, which has been reduced by hundreds of millions of dollars in each round of cuts.
The bottom line is that, because of Medicaid costs, the state will spend more in 2025-26 than lawmakers approved in the 2025 session.
Last week, the House approved the 29 bills in the supplemental budget package.
Most passed with broad support — but not all.
Bills changing the budgets for the departments of state, treasury, health care policy and financing, personnel, public health and environment and higher education all passed largely along party lines.
A supplemental item for the Department of Corrections, which increased its budget by $29 million to account for higher medical costs and more prison beds, got 17 “no” votes from Republicans and progressive Democrats.
The current year’s general fund increased by $171 million, the biggest pot of which — $134 million — comes from the Department of Health Care Policy and Financing, which administers Medicaid.
Overall, the budget for 2025-26 increased by $776 million, with $503 million coming from additional federal funds, almost all of it for Medicaid.
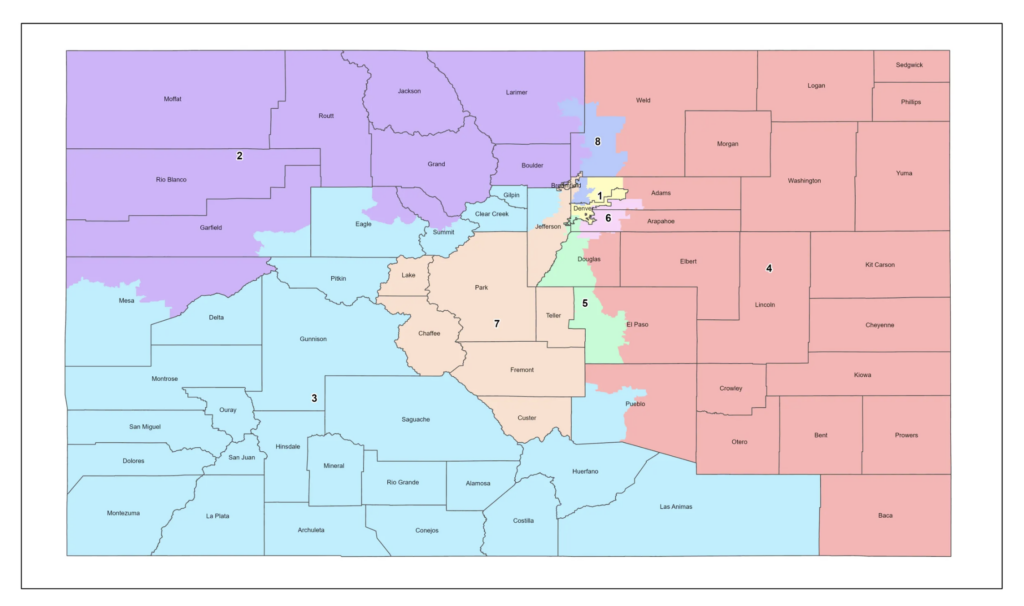
These are costs the state has to pay, said Sen. Judy Amabile, D-Boulder, a member of the Joint Budget Committee that put together the budget package.
Amabile and a fellow JBC member, Sen. Jeff Bridges, D-Greenwood Village, told reporters Tuesday that those extra costs would be paid for from the state’s general fund reserve, which has already been tapped to help cover the budget shortfall that surfaced last August.
“There’s just more and more bad news on top of bad news. And so we have a tough road ahead of us to get to a balanced budget,” Amabile said.
Everything that happens with the supplementals will affect their attempts to balance the budget for the following year, she said.
The reserve, which sat at $2.4 billion at the end of the 2024-25 budget, will drop to $1.85 billion, down about $615 million, to cover those extra Medicaid costs.
“It is responsible to spend the reserve to a certain amount in order to cushion the blow of the cuts that we need to make in a longer term,” Bridges said.
He said he’s working on legislation to raise the Taxpayer’s Bill of Rights limit so that the state doesn’t find itself in the same position in future years. But, he said, “we can’t rely on that” at the moment.
While reserves are there to cover recessions or reductions in revenue, “it is not responsible to spend down your reserves to cover an ongoing fiscal deficit,” he added.
By law, the general fund reserve must be restored to its 15% level unless the legislature votes to reduce it to a lower figure. On Tuesday, JBC members said they’re considering it.
The supplementals, as these bills are called, would implement some of the changes to the budget that began with last August’s special session.
That six-day session was called in the wake of the signing of H.R. 1, a federal bill that legislative Democrats and Gov. Jared Polis said blew a $783 million general fund hole in the current state budget.
Democrats claimed H.R. 1 was responsible for Colorado losing $1.2 billion in income tax revenue, about two-thirds of that from corporate taxes.
Republicans, including at the state Capitol, countered that Democrats have been spending money recklessly, disregarding a structural deficit — meaning there isn’t enough revenue to cover ongoing expenses — that even the governor’s then-budget director began warning about six years ago.
During that six-day session, lawmakers approved bills to generate $253.2 million in corporate tax revenue.
Following the special session, Polis announced $252.5 million in cuts to the state budget, including reductions in Medicaid provider rates, a hiring freeze that lasted until Dec. 31, 2025, and tapping the state’s emergency reserve to cover about $250 million.
Those cuts, as well as tapping the state reserve, had to be approved by lawmakers during the supplemental budget process.
The Joint Budget Committee didn’t approve all of it, so the panel had to find other places to make cuts.
Amabile pointed to an “hour cap” for family providers, part of the health care policy and finance supplemental, as an area where JBC members disagreed with the governor and ultimately decided not to approve. There were additions to the budget the governor sought through the supplemental process that also didn’t win JBC approval, she said.
The Senate Appropriations Committee approved the supplemental budget package on Wednesday.
One of the measures that got the most public attention was the supplemental item in healthcare policy and financing. While the department got a substantial boost in funding to cover escalating Medicaid costs, it also took a hit of more than $54 million, including $17.4 million* in general fund dollars, in Medicaid benefit and eligibility changes in areas, such as funding for drug testing and housing vouchers for people transitioning from nursing facilities to community-based care.
With the Appropriations committee serving as the committee of reference, the public was allowed to testify on the bills, and senators heard from medical providers impacted by the cuts.
Dr. Cassie Littler, speaking on behalf of the American Academy of Pediatrics, pleaded with the committee to amend the bill to restore “access stabilization payments” that go to pediatricians, as well as to rural areas and smaller providers.
Dr. Brigitta Robinson, president of the Colorado Medical Society, echoed that request.
When pediatric practices lose financial stability, the result is fewer well-child visits, delayed immunizations, more emergency room use, and less access to behavioral health, Littler told the committee.
The health care policy and financing plan meant to delay implementation of those payments by six months — to Jan. 1, 2026 — to save $4.6 million, including $1.5 million in general fund dollars. The committee did not make any changes.
Provider rates had been among the hardest hit, with $68 million in general fund dollars cut in more than a dozen areas. The largest, at $38 million, was a 1.6% reduction in overall rates for all Medicaid providers. That put the rates back to where they were in the 2024-25 budget, although leaving out cuts to behavioral health providers and those whose rates are set by federal or state law.
The supplemental budget also cut another $4.6 million in general fund to keep rates paid to Medicaid providers at no more than 85% of costs. It is not an additional cut if the rate drops to 85% once the 1.6% cut is applied.
The Senate is expected to debate the supplementals on Thursday, with a final vote likely by Friday.
Editor’s note: The story has been udpated to correct health care agency budget cut numbers.