Two months after approval of new COVID treatment, many doses have yet to be administered
In November, the Food and Drug Administration announced they’d approved a new treatment that had showed early promise in preventing the most at-risk Americans from ending up in the hospital with COVID.
The federal Department of Health and Human Services told Colorado officials to expect weekly shipments of roughly 1,500 doses of the drug, an IV-infused antibody treatment, said Eric France, the state’s chief medical officer. The treatment was new, and data was limited. But studies had shown it was effective in keeping older or chronically ill Americans with mild-to-moderate COVID out of the hospital. Older Coloradans have accounted for the majority of deaths and hospitalizations here, and when the drug was first shipped in November, the state was facing an unprecedented spike in cases.
In theory, the antibody treatment would’ve been ideal in that moment. France and others expected it to be in high demand, so much so that they created a lottery program to ensure that qualified Coloradans would all have the same shot at getting it, rather than concentrating the doses in big cities or with big hospital systems.
But in a cruel irony of the pandemic, the drug that could’ve helped slow hospitalizations wasn’t widely utilized because hospitals have been too slammed with COVID to jump through needed hoops.
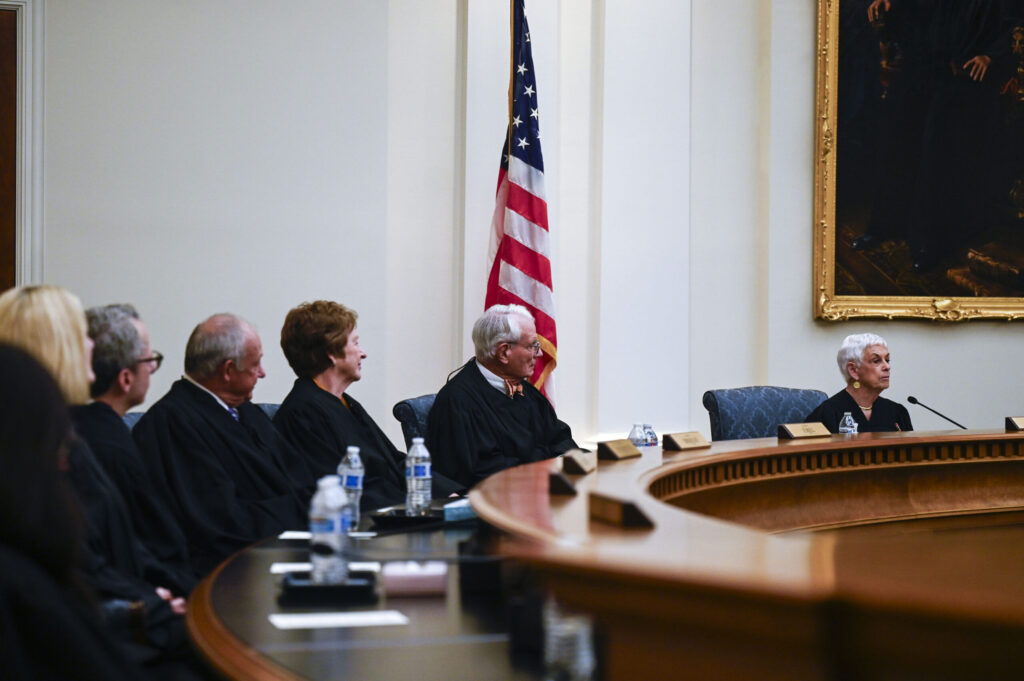
In a mid-December presentation at a National Academies of Science, Engineering and Medicine workshop, France presented slides detailing newfound challenges. His bullet points included one about the length of time needed to set up sites to deliver the drug and about “care delivery systems are saying ‘no thank you'” because they’re “busy with COVID-19 patients.”
As cases climbed throughout November and into early December, as many as a third of Colorado’s hospitals warned that they faced staffing shortages. The state activated previously unused contracts with staffing agencies to bring in more help.
“Many places would say, ‘We don’t want any doses because we can’t free up nurses, we can’t free up staff to go do infusions,'” France said in an interview Thursday. “So there was a staffing concern based on their demands at their hospitals already.”
The result of these obstacles, France said, is that “hundreds of doses” have been distributed, not the thousands that the state has received. The fear that demand would outstrip supply — which led to the creation of the lottery system — has not come to pass. Colorado is not alone in this struggle; as the health care system nationwide has sagged beneath a fall COVID surge, providers across the country have encountered similar obstacles.
France said that after the national academies meeting in December, it was clear that “nobody was getting these doses in arms.”
It’s unclear how many doses of the antibody treatment have been administered in Colorado. Because the Department of Public Health and Environment distributes them to individual hospitals and providers, state officials don’t have an exact count of how many have been delivered thus far.
As of earlier this week, the state had received more than 6,000 doses of antibody treatments. More have been made available to long-term care facilities. The lottery system has been used to distribute just 270 doses. UCHealth said it’s given 125 doses of the drug thus far. Neither of those figures represent exact counts, but are indicative of the limited uptake of the drug thus far.
Now, as the crisis stabilizes, France is working to promote the treatment as a way to head off any future wave of hospitalizations. When the antibody drug first came to Colorado, he and others were hesitant to do too much promotion. They didn’t want to inflate demand on a relatively scarce resource. But now that supply is improved and staffing issues have been somewhat assuaged, he’s turning to improve the demand. If the state can increase the public’s awareness of the drug, and bolster providers’ ability to distribute it, France said, it could help avoid any future strains on the state’s hospital system.
“We’re doing what we can to get the word out,” he said.
When the drug was first shipped, staffing was a paramount concern, and there were more obstacles beyond needing nurses. Infusion centers are dedicated health care facilities that deliver specialty drugs — like chemo or advanced arthritis medications — to patients who often are immunocompromised. These infusions can take a few hours, with the patient sitting in a chair while an IV pumps in their medicine.
Because the patients receiving the antibody treatment are COVID positive, they need their own contained space. Providers couldn’t safely seat a COVID-positive person next to a patient whose immune system has already been battered. That means more space and more staff.
To complicate matters further, the antibody treatment requires not just the hour needed for the treatment itself but an additional one to two hours to monitor the patient for any side effects, said John Hammer, an infectious disease doctor at Rose Medical Center who’s worked on clinical trials for other medications.
“We all know that the risk for infection correlates not only with distance, with space and the use of (protective equipment), but it’s also about time,” Hammer said. “So the increased amount of time spent with an infectious person increases the risk of transmission.”
The distribution of the drug by hospital varied significantly. Paula Freund, spokeswoman for UCHealth, said the system began providing the treatment at “multiple infusion centers” across the state.
“We have given antibody treatments to about 125 ambulatory patients, and so far, we have not experienced any shortages in the drugs,” she said.
Kevin Massey, a spokesman for Centura, declined to comment at all when asked about the system’s use of the antibody treatment. Asked why he couldn’t comment, Massey said that “it isn’t a topic we’re able to discuss at this time.” A spokeswoman for Denver Health did not provide details on that facility’s distribution, either.
Hammer, the Rose Medical Center doctor, said his hospital hasn’t provided any of the treatments. A spokeswoman for HealthONE, Rose’s parent system, said they weren’t providing any of the treatment but may in the future.
Too few staff, too many logistical challenges. But just as consequential, Hammer said, was that the data supporting the drug’s efficacy wasn’t compelling enough for the hospital to jump through the needed hoops.
“I think that what we really need from these agents are more clinical studies,” he said. “The studies on which their (approval) are based involved 200 to 300 people, and they’re really small.”
France has repeatedly acknowledged that the data is somewhat limited. He said that the National Institute of Health concluded “there wasn’t enough evidence for or against” the drug; the NIH announced earlier this week that it’s launching a clinical trial to further evaluate the treatment. Had that robust data been available earlier, France said, then hospitals might have devoted more time, resources and providers to standing up more infusion centers.
But France said that the data does indicate that there is some benefit from the drug, both in keeping patients out of the hospital but also in reducing how much virus they’re carrying around. If it can safely help to stave off the long-feared overrunning of hospitals, then it’s moving in the right direction.
“It feels safe, it looks like it will have benefits, and we’re in the middle of a serious pandemic,” he said.
France is now turning to better advertise the treatment and its availability. Now that the situation facing hospitals has lessened somewhat, more staff should be available and lessons have been learned about how to distribute it. He’s going to speak with providers from the Colorado Medical Society next week and is sending out a message to providers across the state.
Colorado now has 19 infusion centers scattered around the state that can provide the treatment; France said another six can be stood up quickly if needed. If the state’s campaign to inform the public about the drug is successful, France said the lottery system may be turned back on again.
“If we can increase the demand for it by letting citizens and doctors know about it, then if we get to a place where these current programs are feeling a little overwhelmed, that might drive them to open up even more seats (in infusion centers),” he said.