PBM reform in Colorado is about patients — period | OPINION
Few in Colorado, or in this country for that matter, would deny our health care system is confusing and unaffordable for most working families. No one knows that better than Coloradans like myself, managing long-term health conditions we are forced to navigate day in and day out.
As someone living with lupus and serving as the board chair of Lupus Colorado, I’ve seen firsthand how devastating medication costs can be. I’ve lived it personally — standing at the pharmacy counter, stunned as the cost of a medication I depend on suddenly skyrocketed without warning or reason. But it’s the stories I hear from other patients that weigh heaviest on my heart. One woman in our lupus community was doing well on an infusion treatment that truly helped her manage her symptoms and maintain her quality of life. But when the price of the infusion soared, her insurance no longer covered it the same way, and the cost became unaffordable. She was forced to switch to an injectable medication that simply doesn’t work as well for her. Her symptoms returned, her pain increased and she lost the stability she had fought so hard to achieve. It’s heartbreaking — and entirely preventable.
Stay up to speed: Sign up for daily opinion in your inbox Monday-Friday
We all know there is no one silver bullet, no simple solution, to tackle this health care crisis. We can’t only look at one piece of the puzzle, but we can make significant progress piece by piece. A few large pieces of this complicated puzzle that have managed to remain hidden are Pharmacy Benefit Managers or PBMs. However, thanks to the hard work of researchers, journalists, advocates and lawmakers on both sides of the aisle, the role PBMs have been playing in driving up the costs of prescription medications has been brought to light.
PBMs are incentivized to drive up patient costs for medicines because, put simply: They can profit more when patients pay more. The system in which they operate is so convoluted it’s almost impossible for patients and policy experts to understand all of the ways they are manipulating the prices of medications — but that’s where bipartisan House Bill 1094 comes in.
This legislation — which garnered support from lawmakers on both sides of the aisle, local patients, physicians, health policy experts and more — creates transparency in the PBM marketplace and will reduce the costs of critical medications by holding PBMs accountable and prohibiting them from profiting from earning income directly or indirectly based on the cost of a medication. It instead encourages the creation of a flat-fee for service system that will not only provide clarity for carriers and consumers, but also ensure there is competition in the PBM marketplace reducing costs overall.
It’s no surprise there is a lot of deflection and distraction and misinformation being spread to undermine this important piece of legislation. However, facts paint a clear picture. Countless investigations have found instead of working to reduce the costs of prescription medications, PBMs are actually incentivized to increase costs. In fact, the Federal Trade Commission is currently suing the top three PBMs, whose profits grew by 438%, for their role in increasing the costs of insulin.
Far from increasing premiums or health care costs, the nonpartisan Congressional Budget Office found a similar bill to HB-1094 nationally would result in savings of nearly a quarter-of-a-million dollars. West Virginia passed legislation prohibiting PBMs from keeping rebates meant for consumers and a new report posted by the state’s Office of the Insurance Commissioner shows the law cut the average 2025 small-group rate increase by 52%.
Frankly people like myself, and people across the nation are tired of players in the health care industry passing the buck. Whenever meaningful attempts are made to rein in their exorbitant profits the scare tactics of cost increases begin.
This legislation is backed by a large and diverse coalition of patient advocacy groups from Lupus Colorado, to the National Multiple Sclerosis Society, to the Colorado state employee union, and consumer advocacy groups. Failing to act to rein in PBMs now will have real consequences, as we recently saw in Wisconsin when a change in PBM formularies meant a young man couldn’t afford the medication he needed and tragically passed away.
Rather than pointing fingers we need action so patients can afford the medications they rely on to function in daily life, contribute to society and stay alive.
PBM reform in Colorado is about patients — period.
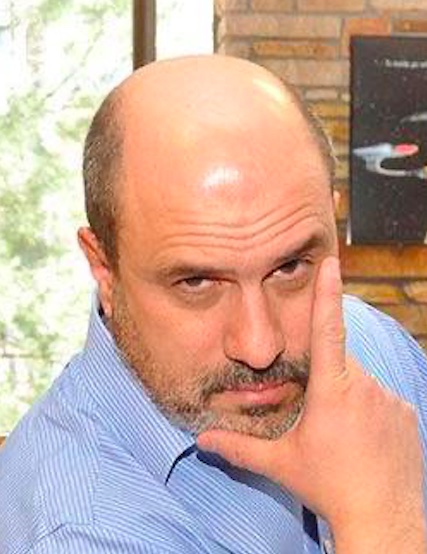
Ron Pierre is a decorated military veteran, Denver law enforcement officer, multi-medal-winning natural bodybuilder and board chair of Lupus Colorado. Diagnosed with lupus at 33, he courageously manages his condition through fitness and nutrition. A devoted husband, father of three and dedicated coach, Ron continues to inspire others through his passion for wellness.