Behavioral health crisis a catalyst for innovation | OPINION


Our nation’s behavioral health crisis is well documented.
The 2022 National Survey on Drug Use and Health, released in November by the federal Substance Abuse and Mental Health Services Administration, found the following:
- 48.7 million people aged 12 or older had a substance-use disorder in the past year. That’s 17% of the nation’s population.
- Almost one in four adults had a mental illness.
For Colorado, these sobering statistics demand we think differently about how we provide health care. We can approach this with urgency by embracing innovative but tested strategies that can provide high-quality care to more Coloradans.
The pandemic and related social isolation contributed to this behavioral health crisis, but it also opened our eyes to the potential of telehealth.
Many of us had little to no experience with videoconferencing technology before the pandemic but now it’s integrated into much of our lives, including often virtual care.
The upsides have been clearly established.
Research shows behavioral health patients are less likely to miss telehealth visits. That’s a benefit to providers, who have blocked out time in their schedules, and for the patients themselves, who experience the continuity of regular care.
Telehealth also provides patients with greater choice when selecting a provider and removes transportation barriers for patients, as they aren’t limited to seeing providers with offices that they must visit in person. This is especially true for those who lack reliable transportation or have limited mobility. In more sparsely populated areas, transportation to providers can be a significant barrier to health care access.
Stay up to speed: Sign up for daily opinion in your inbox Monday-Friday
Many patients using telehealth do so from within their homes. In doing so, providers gain a glimpse into where their patient lives and can provide valuable clues about a patient’s condition that would not be as evident from a session in the therapist’s office. For instance, is their home environment orderly or chaotic?
Long before the telehealth era, I saw a long-term psychotherapy patient who moved overseas. For a few months until she was able to find a local provider in her new home, our psychotherapy sessions were conducted by telephone. As her psychiatrist, it required me to be extra attentive, listening for changes in intonation, for example, in the absence of visual cues.
Just like the innovation of TV provided a more complete picture than radio, the advent of video calls has made virtual therapy more effective.
For mental or physical care, telehealth isn’t always the best fit. Local providers offering in-person visits will continue to serve as the backbone of a robust network. Telehealth can be a beneficial supplement if used in appropriate situations to expand care.
Increasingly, we’ve come to understand the extent to which behavioral health and physical health are interconnected and how care needs to be integrated.
One emerging approach that recognizes this mind-body connection, and how to treat a patient holistically, empowers certain behavioral health providers to serve as primary care providers.
The sad reality is people with serious mental illness have been shown to have substantially reduced life expectancy. This is often due to untreated or poorly managed physical health conditions such as cardiovascular disease, diabetes or hypertension.
A qualified mental health clinician would rarely serve as the sole provider but could coordinate the rest of the patient’s care team to reduce the patient’s risk of complications from physical health conditions. For people with a substance use disorder who benefit from medication-assisted treatment, this has been shown to be a particularly effective model.
Throughout the history of our nation and our state, periods of upheaval have served as catalysts for innovation. Colorado’s behavioral health crisis can bring out the best in our state as we rise to meet this great challenge, but only if we seize upon this opportunity to view telehealth as a critical component to addressing our behavioral health workforce shortage, and to help in delivering this care that is so vital.
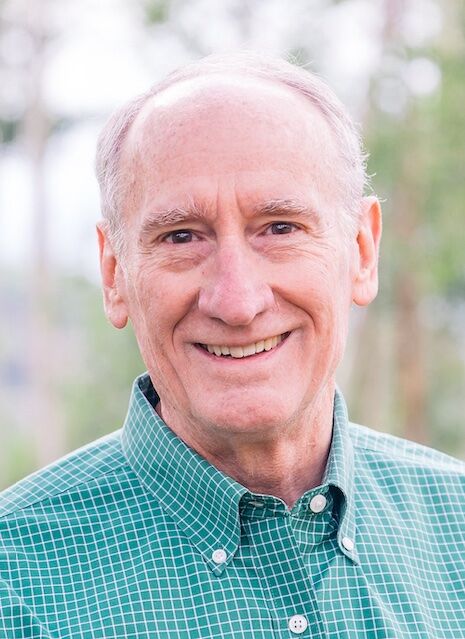
Patrick Fox, M.D., is president of Colorado Medicaid for Elevance Health, a Colorado Community Health Alliance partner.