Colorado bill seeks to limit step therapy in serious mental illness treatment

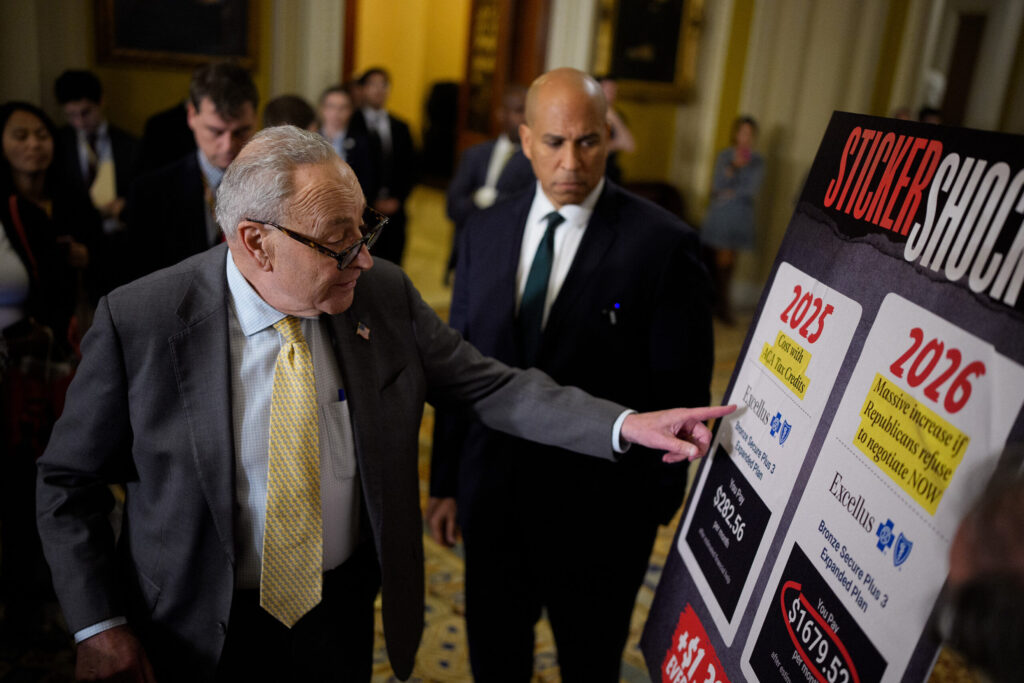
When a doctor prescribes medication for a patient, insurance companies often require the patient to first try a series of alternative, less expensive drugs before they will cover the originally prescribed medication.
Critics say that process – called “step therapy” – delays lifesaving care.
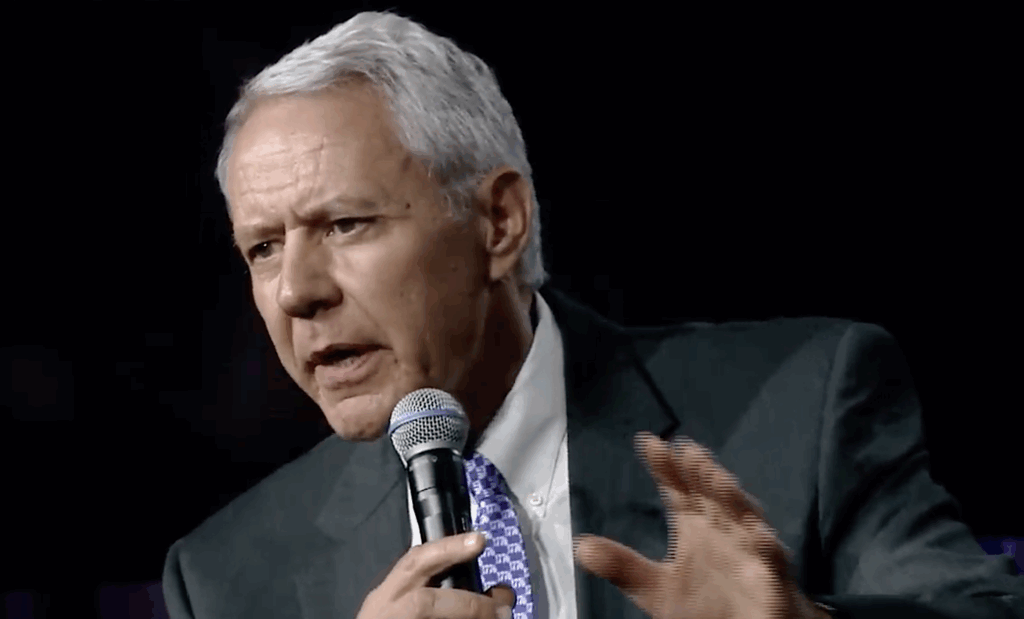
Rep. Dafna Michaelson Jenet said when she was diagnosed with major depressive disorder, she was forced to spend weeks taking multiple ineffective drugs that only worsened her mental health.
“The drug that I’m taking today has been an absolute game changer in my life. The drugs that I had to take left me suicidal, left me unable to get out of bed and left me unable to function,” said Michaelson Jenet, D-Aurora. “I had to go through that process and, as a result, I lost weeks of my life. And I will never get those weeks back.”
Michaelson Jenet is now sponsoring House Bill 1130, which seeks to limit step therapy requirements when treating serious mental illnesses.
If approved by the state legislature, the bill would only allow commercial insurance providers to make a patient try one alternative drug before covering the medication originally prescribed by the patient’s doctor when treating depressive, bipolar, psychotic, schizoaffective and obsessive-compulsive disorders.
The bill unanimously passed its first committee vote on Tuesday.
“This process of forcing patients to verify that other drugs are ineffective or inadequate drives every doctor crazy,” said Amy Goodman with the Colorado BioScience Association. “This can prolong and worsen health issues, needlessly subject vulnerable patients to serious side effects and ultimately cause patients to abandon seeking treatment altogether.”
Goodman and other proponents of the bill said the use of step therapy is dangerous for Colorado patients as the state is in the midst of a mental health crisis.
In 2022, 23% of Colorado adults had some kind of mental illness, but only 55% of them received treatment, according to a State of Mental Health in America report. Nationally, 42% of Americans say cost and poor insurance coverage are their top barriers to mental health treatment, with 17% saying insurance does not pay enough for their mental health treatment, according to a 2018 study.
More than a dozen organizations back the bill, including the Colorado Hospital Association, Colorado Behavioral Health Care Council, Colorado Medical Society and the National Alliance on Mental Illness. Only the Elevance Health insurance company opposes the legislation.
The Pharmaceutical Care Management Association also supports the bill, though it defended the use of step therapy. Patrick Boyle with the association said his group is only supporting the bill because it allows insurance companies to keep one step and was amended to not take effect until 2025.
“The reason we have step therapy is, regrettably, cost is a consideration in the provision of health care,” Boyle said, giving an example of two different drugs that treat autoimmune disorders that cost $70 per month and $7,000 per month.
“We can either treat 100 people … or one,” he said.
Step therapy can reduce costs for insurers by between 9% and 15%, according to some studies. However, other research shows that step therapy can impede patient health and increase long-term costs, particularly for patients who require hospitalization due to the alternative drugs – as Michaelson Jenet did.
The House Health and Insurance Committee unanimously approved the bill Tuesday, advancing it to the House Appropriations Committee for further consideration.
If passed into law, the bill, which would take effect on Jan. 1, 2025, would also require the state’s medical services board to review new mental illness medication for coverage within 90 days of federal approval.
During the committee hearing, Rep. Karen McCormick, D-Longmont, said the bill is “a great first step” in getting rid of step therapy. Rep. David Ortiz, D-Centennial, called step therapy “insidious,” saying he was told to take a wet wipe bath instead of getting bathroom chairs as step therapy for his disability coverage.
“This bill is lifesaving,” Michaelson Jenet said. “When dealing with serious mental illness, time is absolutely of the essence. What I’m asking for here is a little less time between the patient and the medicine that works.”