Colorado medical experts approve update to crisis triage plans
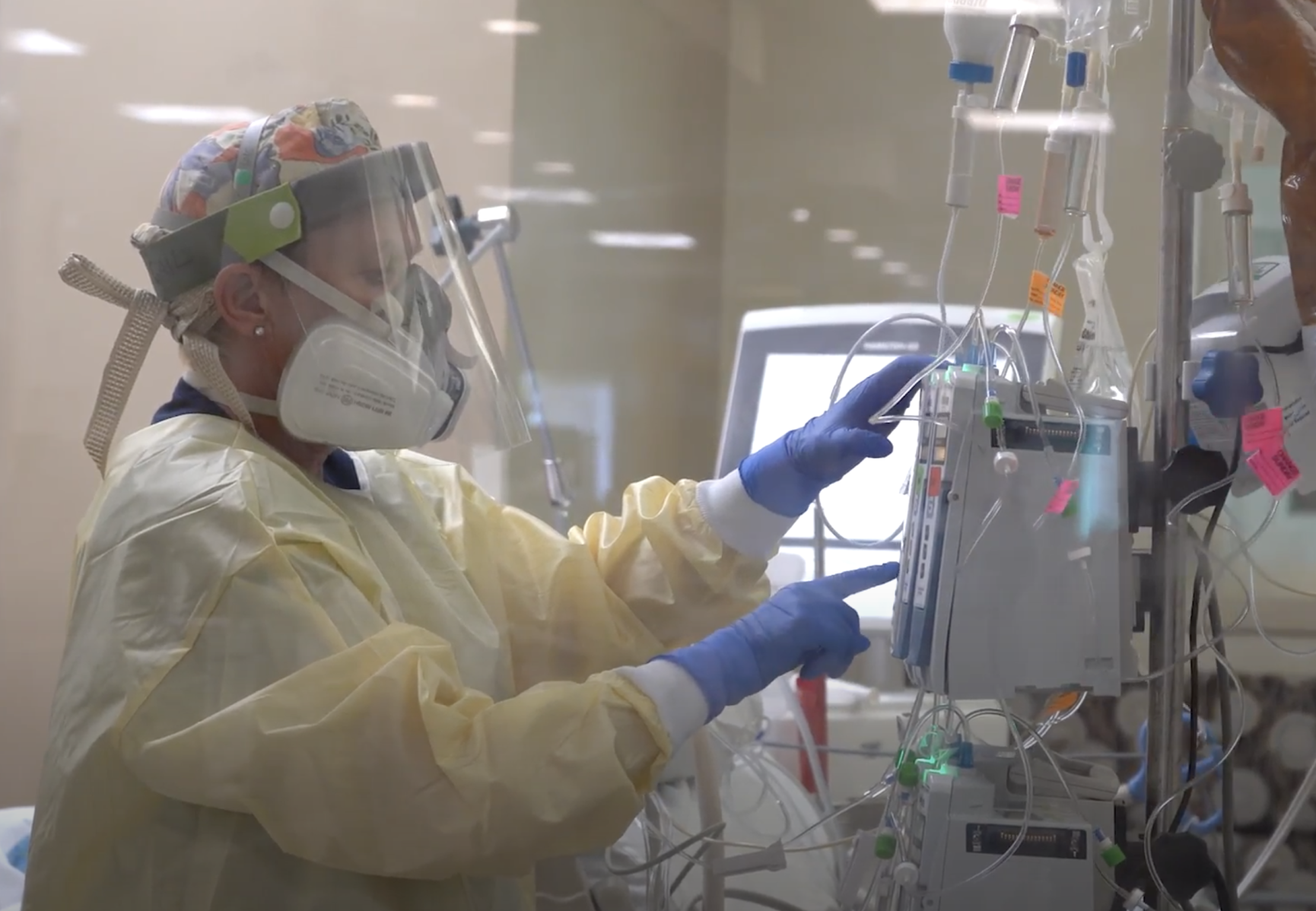
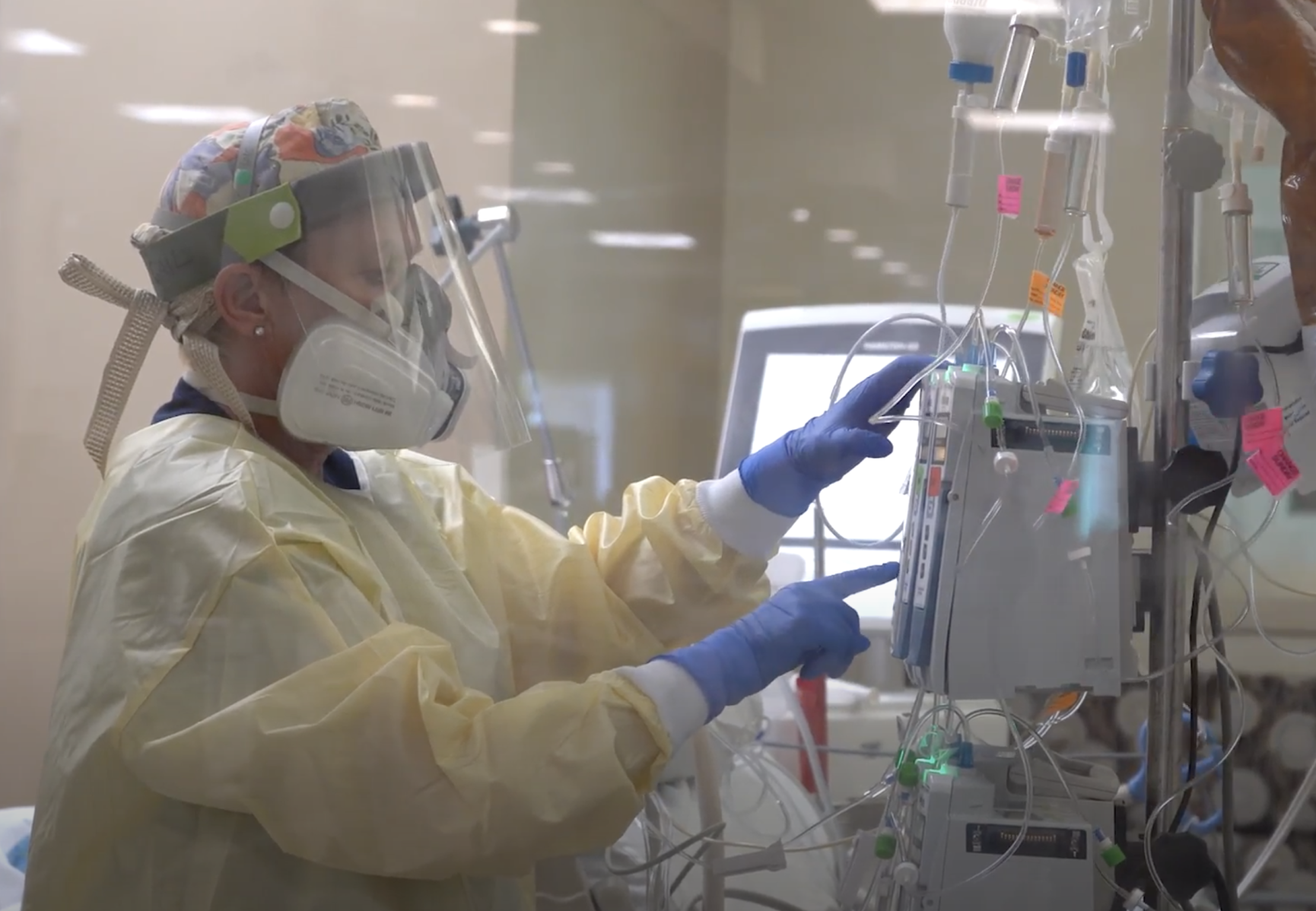
If overwhelmed, Colorado hospitals would be able to turn away and approve early discharges for patients who are deemed safe to go home and seek care elsewhere, according to a crisis plan finalized by a team of medical experts Monday.
The unanimous vote by the group does not activate the plan, a critical piece of the crisis standards of care. It instead sends a final version to Gov. Jared Polis for approval, after which point the governor can trigger it should Colorado’s hospital capacity be overwhelmed. The document, an update of a plan approved last year, details guiding principles for hospitals to follow should they have to ration care and decide who needs a hospital bed and who doesn’t. Though some parts of the plan have been activated – like those governing staffing – Colorado has not had to begin rationing care to this worst-case degree.
The plan, if ever activated, would apply to all hospital patients, not just those with COVID-19. Vaccination status is not a factor that will be considered when making triage decisions; earlier this month, several members of the team drafting the standards flatly opposed such a consideration.
Anuj Mehta, a Denver Health physician who led the drafting process, said that the “psychological distress” caused by even considering a triage scenario is “extreme.” But given the state of Colorado’s hospitals, which at some points in recent weeks have had fewer than 700 beds available, members of Polis’s Expert Emergency Epidemic Response Committee moved swiftly this month to update the plan.
If hospitals got to the point of being overwhelmed, Mehta continued, even a 10% “decompress” in patient volume via the standards would be “a boon” to providers and the health system.
The previous version of the plan would weigh a patient’s likelihood of survival in deciding if he or she should get one of a limited number of ventilators or other treatments. That piece is still part of the plan, Mehta said, but the larger focus is on patients whose care can either be stepped down – from an intensive care bed to a standard medical-surgical, for instance – or relegated to outpatient facilities, like a primary care or specialty physician.
A patient could enter the emergency room, for instance, with chest pain. That patient’s status would be evaluated by a triage team and a scoring system, which would weigh various factors to help determine a patient’s prognosis. Depending on that evaluation, the patient could either be sent home to seek outpatient care, or they could be admitted to a bed.
The same system would be used for a patient already admitted. Using a similar system, a patient may be discharged early should he or she be well enough to go home and get care elsewhere.
Mehta said the standards would identify the “lowest-risk patients” who were not only well enough in that moment to go home but would also be less likely to return to the hospital in the near future. The patient’s survivability could also be taken into account: “Is the patient going to pass away, unfortunately, even if they receive a ventilator?” he said.
Given the needed emphasis on the ability of patients to seek care outside of the hospital, Mehta said socioeconomic factors must be considered in those decisions. A person living on the street, for instance, could not be referred to outpatient care. The same is true for an uninsured patient or other vulnerable populations.
As a result, Mehta said the plan would inevitably give priority to the most vulnerable patients, rather than relegating them to the back of the line. Older people or people with disabilities may not be able to care for themselves at home and thus need a hospital bed.
“In those settings, these patients would be prioritized for inpatient care because they don’t have access to standard outpatient therapy,” he said, adding that hospitals and the state would need to conduct constant evaluations to ensure one demographic group wasn’t being disproportionately affected by the standards.
No member of the committee – which included local and state health officials as well as individual hospital leaders and physicians – criticized or spoke against the plan. Dan Pastula of UCHealth said the document was “as logical and fair a document as I can think of under the circumstances.”