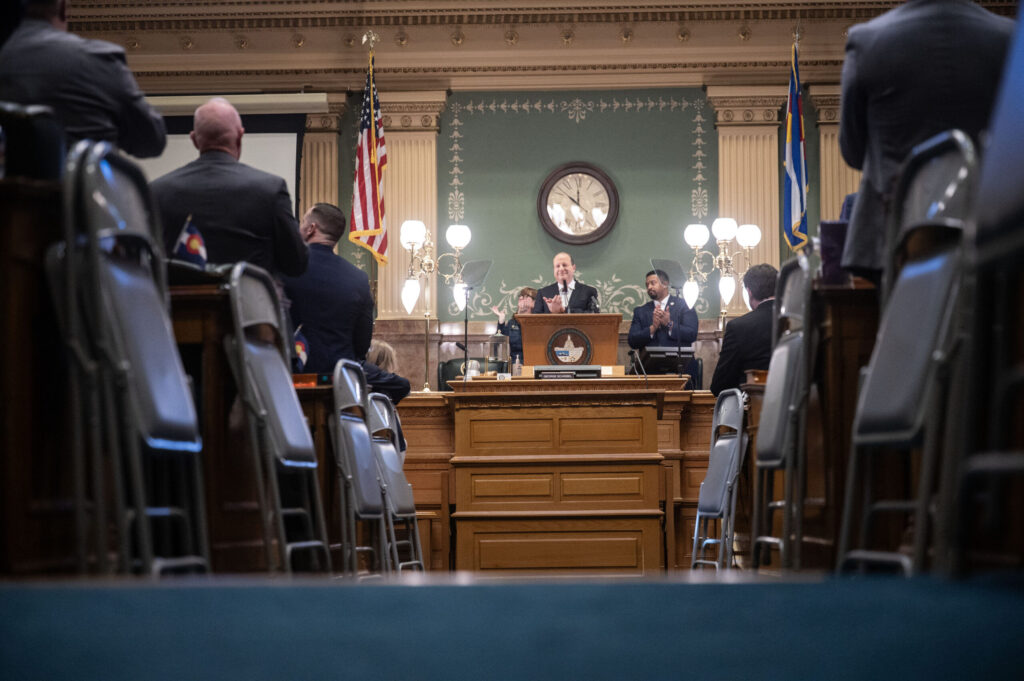
Lawmakers, Gov. Jared Polis clash on Medicaid provider rates

Colorado legislators on Tuesday heard from an advisory committee, which proposed making several adjustments to the state’s reimbursement rates for health care facilities that provide services to Medicaid patients.
The proposal from the Medicaid Provider Rate Review Advisory Committee diverged from Gov. Jared Polis’ own proposed changes outlined in his budget proposal for the next fiscal year.
Megan Adamson, chair of the advisory body, said the committee has been meeting with Medicaid patients, providers and others to discuss concerns and suggestions. Of more than 200 instances of written and verbal feedback, most focused on outpatient physical, occupational, and speech therapy services, neuropsychological testing, and dental care for individuals with intellectual and developmental disabilities.
For its recommendations to the Joint Budget Committee, the advisory body used Medicare reimbursement rates as a benchmark and looked at data from other states when no Medicare rates were available.
For the majority of services — including dialysis, prosthetics, vision care, dermatology, gynecology, and neurology — the committee recommended that the state increase payments to up to 80% of the Medicare benchmark or maintain rates at the current 80% level.
For codes that do not have a Medicare equivalent, the group recommended increasing rates by 3% to adjust for inflation.
Based on feedback, the body also recommended increasing rates for certain “high impact” services, such as dental care for individuals with disabilities and neuropsychological testing. For those codes, the body recommended increasing rates that are below 100% of the Medicare benchmark up to 150%.
In addition, the advisory body presented several policy recommendations for the state’s Department of Health Care Policy and Financing, including adding coverage for exome sequencing, ensuring parity between reimbursement rate structures for physical, occupational, and speech therapies, and using a specific code marker to identify services being offered in primary care settings to “incentivize or enhance” those payments.
The total estimated cost of the recommendations is about $26 million, nearly $9 million of which would be from the state’s general fund.
Last week, Polis met with the Joint Budget Committee to discuss his proposed budget, which included nearly $200 million in general fund dollars for the state’s Medicaid program. That amounts to about 5.6%, though the program’s projected growth is about 11.9%, which translates to more than $631 million.
Polis told the Joint Budget Committee that Medicaid is the fastest-growing portion of the state’s spending – growth that, he said, isn’t sustainable.
While the majority of JBC members pushed back on Polis’ plan, they didn’t appear to like what the Medicaid Provider Rate Review Advisory Committee recommended, either.
Several lawmakers wondered how the advisory body came up with the 80% benchmark figure, especially when the Polis budget proposes cutting all provider codes to 85% of Medicare rates.
Sen. Barbara Kirkmeyer, a Republican from Weldy County, wondered if the governor’s reimbursement rate structure negated the Medicaid Provider Rate Review Advisory Committee’s recommendation.
“It definitely is a significant challenge,” said Adamson. “The biggest challenge across the board is that it doesn’t allow us to be thoughtful about what areas are going to be most impactful for the individuals in our state.”
It also makes it very hard for providers to make “predictable decisions” amid workforce shortages and insufficient funding, she said, adding, “It is important to stick with a rate review process that allows us to be thoughtful.”
Sen. Judy Amabile, D-Boulder, also questioned whether there is any data proving 80% of the benchmark is the best figure, as opposed to something like 75% or 85%.
Adamson said the body typically recommends reimbursement rates between 80 and 100% of the Medicare benchmark, adding anything below 80% would be too low. Adamson and her colleagues have been “somewhat reluctant” to cut rates any further, as they fear it could reduce access to care, she said.
“We hear the challenges that providers have in continuing to accept Medicaid when those rates get too low,” she said.
When reached for comment, a spokesperson for the Governor’s Office said Polis “submitted a responsible, balanced budget proposal that fully funds schools, funds public safety improvement and increases funding for Medicaid to record levels to ensure that our most vulnerable Coloradans continue to have access to the care they need and deserve, now and in the future.”
Marianne Goodland contributed to this story.