Protect Colorado patients from dangerous care delays | OPINION


Cancer is one of the leading causes of death in the Centennial State, with approximately 25,000 Coloradans diagnosed with the disease – and roughly 7,600 dying from it – each year. For these patients, timely access to specialty drugs, therapies and treatments is critical to their survival.
As a medical oncologist and hematologist for more than two decades, I’ve dedicated my life to providing the highest-quality care to my patients. This means ensuring cancer patients can access chemotherapy and other essential treatments in a safe, efficient manner.
Unfortunately, so-called “white bagging” mandates put in place by insurers and Pharmacy Benefit Managers (PBMs) cause dangerous delays in treatment for Coloradans battling cancer.
It is standard practice for community oncology clinics to manage an on-site drug inventory to provide personalized care. When a patient arrives at their appointment, I evaluate their treatment progress and adjust their chemotherapy based on disease response or side effects. With an on-site drug inventory, I can make modifications to provide effective care and can ensure tracking of the drug’s chain of custody, ensuring the integrity of the product.
Stay up to speed: Sign up for daily opinion in your inbox Monday-Friday
White bagging mandates, however, require oncologists to order the chemotherapy from specialty pharmacies owned or affiliated with large insurers. This disruptive process boosts insurers’ profits at patients’ expense. For oncology treatments, white bagging mandates save insurance companies an average of roughly $2,100 per patient per month, with no discernible reduction in patient premiums, while increasing out-of-pocket costs for cancer patients by about $170 per month.
Though my practice has banned white bagging due to safety risks, many of my colleagues from Denver to Durango are subject to these mandates, which add unnecessary, life-threatening complexity to an already difficult treatment process.
Once a white-bagged drug arrives, it can only be used by that specific patient, meaning practices must manage a separate inventory for each patient and insurer. Many drugs start to degrade shortly after being mixed, so if that patient can’t get the drug on time, it must be destroyed.
If one of my cancer patients were to experience a negative reaction to a drug, I would have to wait for the specialty pharmacy to mail the corrected dose – even if that exact same drug was sitting in my on-site inventory. Not only does that waste patients’ travel time, time off work, or childcare arrangements, it also results in lengthy delays that allow a patient’s disease to progress.
The white bagging process also introduces a range of safety concerns. Community oncology clinics can monitor the temperature, storage and handling of each drug prior to administering it to a patient. However, a white bagging process cannot ensure these safety protocols are followed.
Despite these risks, white bagging policies and practices are accelerating. In a recent poll of Association of Community Cancer Centers (ACCC) members, more than 87% report “white bagging is an insurer mandate for some of their patients.” Without action from policymakers, this trend will only continue, jeopardizing the health and safety of Coloradans fighting to overcome cancer.
Fortunately, state Reps. Iman Jodeh and Matt Soper, along with state Sen. Dafna Michaelson Jenet, are leading the charge to restrict this harmful practice in Colorado. I am grateful to them and to our national partner, The U.S. Oncology Network, for their work on HB 24-1010 which will help protect and strengthen Coloradans’ access to care.
This legislation would prohibit insurers and their affiliated PBMs from requiring patients with chronic, complex, rare or life-threatening medical conditions seeking care in community practices to receive their physician-administered drugs from a specialty pharmacy. In doing so, it would help ensure cancer patients are getting the timely, personalized care that gives them a better chance at recovery and remission.
States around the country, including Texas and North Dakota, have already taken action to pass similar legislation that restricts white bagging. It’s time for Colorado lawmakers to follow their lead and rein in this harmful practice.
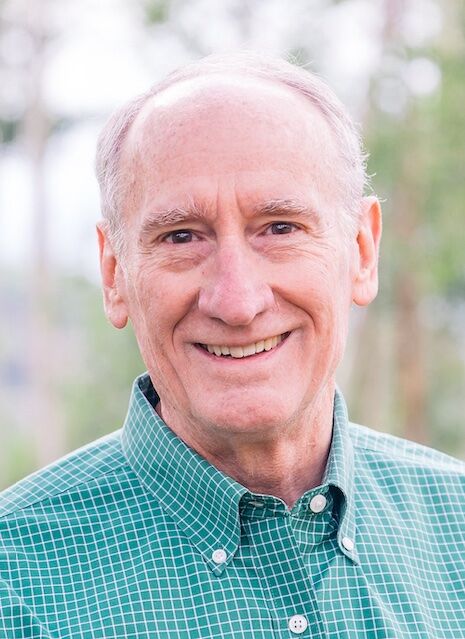
Dr. Leslie Busby is a board-certified medical oncologist and hematologist at Rocky Mountain Cancer Centers practicing in Boulder. As the chairman of the U.S. Oncology Network Pharmacy & Therapeutics Committee, Dr. Busby is directly involved helping practices like Rocky Mountain Cancer Centers provide safe and efficient therapy in their practices and bringing the most recent advances in cancer therapies to patients.