Monkeypox in Colorado: No community transmission found, state officials say
Colorado officials have not detected any community transmission among the handful of monkeypox cases identified here thus far, and the bulk of people exposed to the virus have been health care providers who’ve treated infected patients.
Five monkeypox cases have been identified in the state – three definite and two awaiting federal confirmation.
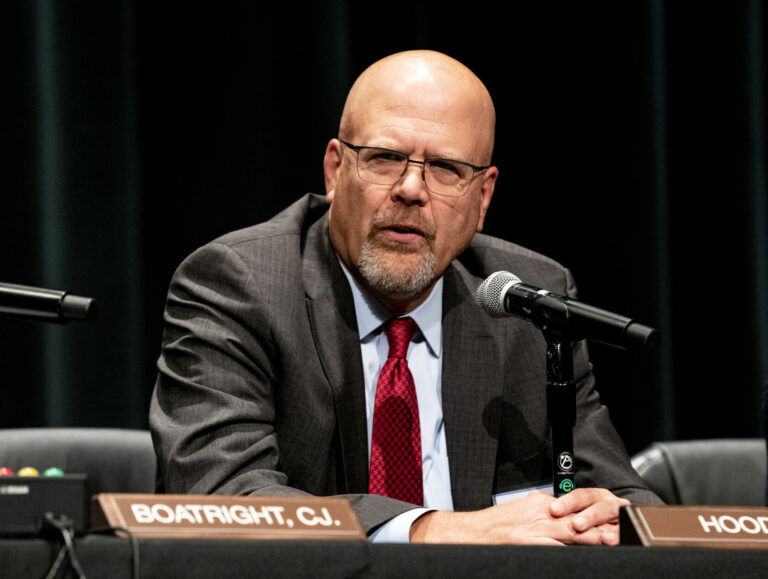
All of those cases have been among international travelers and men who identify as having sex with other men, state epidemiologist Rachel Herlihy told reporters Wednesday, and as such, the virus does not pose the same threat as that presented by COVID-19.
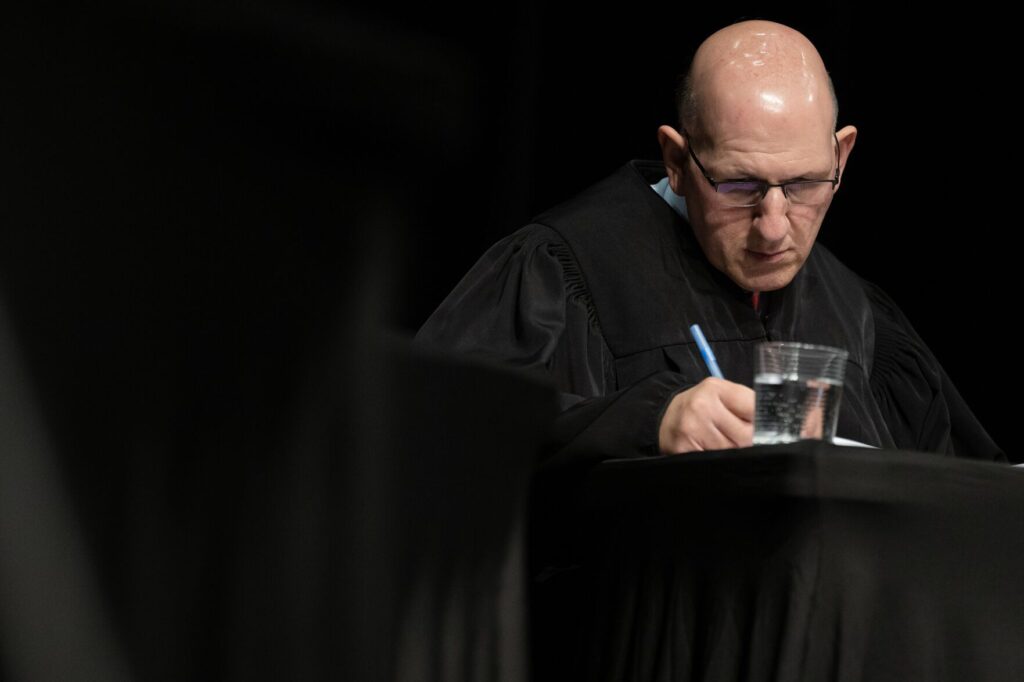
Scott Bookman, the state’s COVID-19 incident commander, said monkeypox was a “very different situation” than COVID. None of Colorado’s cases has required hospitalization. Cases that required hospital stays elsewhere were primarily for pain management, Herlihy told the state’s board of health last week.
Providers begin vaccinating young Coloradans days after federal green light
“This virus is not nearly as transmissible (as the virus that causes COVID-19),” Bookman said. “We are not seeing widespread transmission at this point.”
Herlihy told the state’s health board that monkeypox is caused by the same family of viruses that causes smallpox. She said monkeypox is the “most significant” of that viral family “since the eradication of smallpox”; it’s typically isolated to African nations where animals act as reservoirs. The smallpox vaccine, she continued, provides protection against monkeypox, and waning immunity from that inoculation may be a factor in what’s driving the international spike in monkeypox cases.
As of June 15, when Herlihy spoke with the health board, 35 Coloradans were being monitored for symptoms after exposure to an infected person; twenty-six of those people are health care workers.
Report: Southeastern Colorado residents face highest health risk from climate change
Typically, the condition improves without treatment. But the state has also received a small amount of vaccine that can be used on people who were exposed to the virus, to lessen their chances of contracting it, or have been infected with it, to improve their outcome. Twenty-four Coloradans have received the vaccine after being exposed; at least 13 of those are health care workers.
Herlihy told the health board that the exposure risk to health care workers is related to the use of protective gear. She said the state was working to improve awareness, via webinars and health alerts, to ensure providers are wearing appropriate gear when treating potential monkeypox cases.
But the challenge, she continued, is that early symptoms of the disease are non-specific; even the rash that accompanies it can be confused with other common ailments. Some people infected in this latest global spike have shown no onset of fever or other symptoms before the rash appears.
At Wednesday’s news conference, Herlihy told reporters that close contacts for monkeypox are different from COVID-19, where relatively brief interactions can still lead to transmission. She said skin-on-skin contact qualifies, as does prolonged interactions, such as among people who share a household. Infected linens can also cause monkeypox to spread, though she said that’s “less common.” She told the health board that passing exposures in places like grocery stores aren’t very likely to spread the disease.
The state lab is processing a handful of monkeypox tests each week, Herlihy said, and it has supplies to last several weeks at the current testing rate. Should that not be sufficient, she said, the state will go to the Centers for Disease Control and Prevention to get more.
Herlihy said health officials across the country and globe are trying to determine if the virus has the ability to become endemic, or if its transmission can be sufficiently suppressed to prevent it from regularly spreading from person to person. There are also conversations occurring about the future role of vaccines: because supply is limited, it’s only being used on people who were exposed to the disease. But, she said, “there might be a shift” toward more preventive inoculation in the future.
She urged people to answer the phone when public health investigators call or to return their calls if they’re missed. All information is kept confidential, and those interviews are key to helping the state control spread. Anyone exposed to the virus should seek testing, she said.