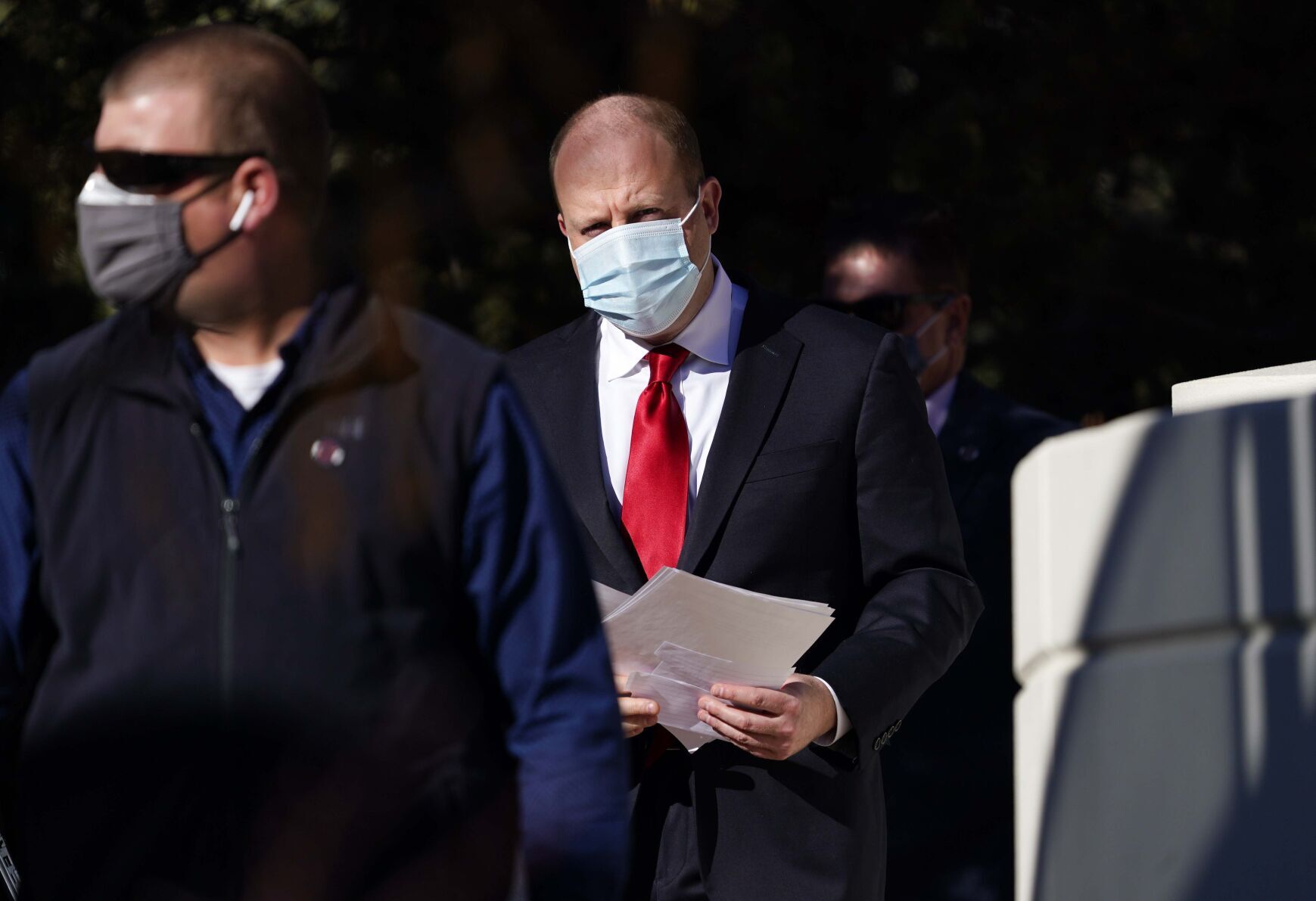
Colorado hospitals, nursing homes need hundreds more staff to meet Gov. Jared Polis’ 500-bed surge goal
Colorado’s hospitals and nursing homes will need hundreds of additional staff in the next month to meet Gov. Jared Polis’ goal of adding 500 hospital beds by mid-December, industry officials said Thursday.
Colorado has the health infrastructure to add the needed beds, officials say. What’s missing are the staff.
State leaders say they plan to tap federal medical providers, out-of-state contractors and retired medical workers to reinforce the state’s depleted health care workforce. The effort will be multifaceted, Polis and Scott Bookman, the state’s COVID-19 incident commander, said this week: Not only will hospital capacity be studied and expanded, but staffing in nursing homes will also be targeted, allowing those facilities to take more discharged patients and free up hospital beds.
But to provide sufficient staffing to man the needed beds, hundreds of providers must be brought in quickly, hospital and nursing home officials said Thursday. Staffing shortages have increasingly plagued the health care system as the pandemic has dragged on, to the point that there are hundreds fewer hospital beds available now compared to a year ago. The state this week moved to ease limitations for staffing to stretch what’s currently available.
Facing similar problems, Colorado’s nursing homes have roughly 2,000 fewer beds now than they did pre-pandemic, constricting hospitals’ ability to move some patients and free up their own space.
“I’d say it’s 500 providers to get to 500 beds (in nursing homes),” said Doug Farmer, who heads the Colorado Health Care Association, a nursing home trade group. He said there were roughly 400 hospital patients who would qualify for nursing home transfers as of two weeks ago.
“I would suspect that actually finding 500 staff members in this environment is going to be near impossible,” he added. “But I don’t know that for sure. I don’t know what exactly their plan is.”
Bookman told health officials Wednesday that the state was “moving as rapidly as we can” and had an “enormous amount of staffing contracts coming in.” Cara Welch, spokeswoman for the Colorado Hospital Association, said the state will foot the bill for those traveling providers, the costs for which have spiked. More providers, provided by the federal government, are also being pursued. One has already been deployed, and at least two more have been requested.
Where those additional providers are needed and deployed may fluctuate: If hospital staffing increases, for instance, more beds can open in those facilities and fewer would be immediately needed in nursing homes. Regardless of where they end up, hundreds of providers are needed if Colorado is to meet Polis’ goal of surging capacity by mid-December, when Colorado is expected to near 2,000 COVID-19 patients. That would mark the worst point of the pandemic thus far.
Welch agreed that it would take hundreds more providers between hospitals and nursing homes to meet the governor’s goal. She said hospitals are at the limit of their surge capacity with the resources they have now.
As of Thursday, there were fewer than 700 total hospital beds left in the state, including just 72 intensive care beds. (Hospital officials have cautioned that available bed capacity can change quickly, as patients are discharged and facilities shift resources.) Space is not the issue, Welch and other hospitals have said. It’s staffing.
Welch said the state is also studying opening up existing facilities – such as closed hospitals or outpatient centers – to expand capacity. But that remains contingent on staff. Right now, large overflow sites are not in immediate plans; if staffing were addressed, space is available within current facilities.
Bookman, the state incident commander, said Wednesday the state wants to “capitalize on infrastructure that exists” rather than “creating free-standing alternate care sites,” like those stood up in spring 2020.
Lindsay Radford, spokeswoman for Centura, said the system has “the ability to assist with the increase of beds across the state,” such as by opening Centura’s bed tower at St. Anthony North campus. That’s assuming, though, that “there is staff available to support this extra bed capacity.”
Radford said Centura was not aware of Polis’ 500-bed announcement before he publicly unveiled it Wednesday. (In a statement, Bookman said the state was in “constant and regular contact” with the hospital association and various system officials.)
Connie Price, the chief medical officer of Denver Health, said she wasn’t aware of the exact numbers Polis wanted before his announcement. Denver Health is at capacity, she said, and has requested federal provider teams, one of which has already deployed in Pueblo, to help alleviate pressure there.
“We do have a plan for additional beds that was developed during the first wave that we could be ready to deploy,” Price continued, “but we have new issues now with staffing that we did not have earlier in the pandemic.”
Asked if it would be possible to surge in time, Welch said, “We have to.” She “put it in the hands of the state” to find the needed providers.
“We’re hopeful; we’ll be working with (state officials) on it to do our best to make it happen,” she said. ” … I think we’re at a point where we don’t see the cases or the hospitalizations declining in the near future, so we have to move full steam ahead with these big plans to have the capacity we’re going to need.”













