Medicaid spending surge for therapy sessions prompts Colorado to reinstate limits

Colorado’s health agency will reinstate prior authorization requirements for Medicaid patients’ therapy sessions next year as part of its efforts to control costs, which soared following a state law passed in 2022.
That year, the state legislature adopted a bill prohibiting health plans from requiring prior authorization for psychotherapy sessions for Medicaid recipients. While the bill was intended to remove barriers to accessing mental health and treatment for addiction for disabled and low-income Coloradans, it increased the amount the state was spending on Medicaid by nearly 75%, according to Cristen Bates, the director of Medicaid and CHP+ Behavioral Health Initiatives and Coverage.
In an August meeting, Bates said there are several reasons why the state’s Medicaid spending has gone up so sharply in the past half-decade: The state expanded its network from about 6,000 providers to more than 13,000, increased provider rates, and added dental and vision benefits. The state also received a 1115 waiver for addiction treatment in 2021, which allows waiving certain Medicaid requirements to test new programs.
Reflecting on the 2022 law, Bates said that, initially, the program expected to “make things a little bit easier” by removing administrative burdens. Instead, the department found itself facing an unexpected $40 million increase in Medicaid spending for behavioral health and substance abuse.
Bates explained that the spending increase was primarily driven by a small percentage of patients who received significantly more therapy sessions than average. She argued that if someone is needing more than one therapy session per week, it could indicate a need for a higher level of care or a different form of treatment.
“We really need to reevaluate what services people need and how much quality they’re getting,” she said.
Another major cost driver is the state’s peer services program, which connects individuals struggling with substance abuse or mental health issues to peers with similar experiences. While the program has been effective at preventing hospitalizations, associated costs have increased by 95% each year since 2021, Bates said. A key factor is the absence of limits on daily billable hours, resulting in some clients billing up to eight hours of peer services treatment each day.
Bates told Colorado Politics the state has seen a 98% increase in the number of Medicaid patients receiving more than 56 therapy services a year. While this may be appropriate for “a small number of people” with complex issues like PTSD or those for whom medication is not effective, she believes there are other patients who are receiving far more treatment than medically necessary.
“When somebody is sitting there taking 40 sessions, that means the next person is waiting in line and not getting care,” she said. “So, there’s the workforce issue here of needing to make sure that therapists are serving more people, and we need people to get more access and go complete the programming.”
“It’s not about whether the client wants therapy, it’s whether or not the therapy is actually medically necessary for a specific disorder,” Bates added.
To combat excessive spending, over the summer, limits were placed on which providers can administer peer services. The agency has also collaborated with regional entities responsible for administering Medicaid services at the regional level to educate and train providers on Medicaid requirements.
Seeing the need to cut more spending, the agency implemented a number of changes last month, including the prior authorization requirement.

‘We opened up the gate really wide, and we didn’t really build a fence around it‘
Behavioral health spending in Colorado has increased “significantly,” Bates said, particularly following the creation of the Behavioral Health Task Force in 2019.
“(Health Care Policy and Financing) said, ‘listen, we’re having some big challenges statewide, and we need to have a focused intervention to say we are trying to expand access to care, improve care quality, and improve the type of care people get,'” she said.
Following the dissolution of the task force, the state expanded its Medicaid coverage to include peer support programs, medication-assisted treatment, residential, and partial hospitalization programs for substance abuse disorders.
These changes led to a “huge” increase in hourly therapy services, Bates said, adding some were legitimate, and some not so much.
“We opened up the gate really wide, and we didn’t really build a fence around it, so we really needed to identify where these planned increases were happening, and where is there just outright fraud?” she said.
“I do think there were some consequences to really significant expansion of benefits of networks of providers. Some of them are just getting providers used to working with Medicaid, and it is difficult and there are additional administrative requirements, but I do think a lot of providers want to serve people who are in lower-income populations and they don’t want to limit their practice to only cash (payments),” Bates added. “I think that ethically, there’s a lot of providers who want to do that, but we need to train them.”
The majority of instances of Medicaid fraud and abuse seem to be occurring at smaller, newer providers who may not have as many resources or experience with serving the Medicaid population, Bates said.
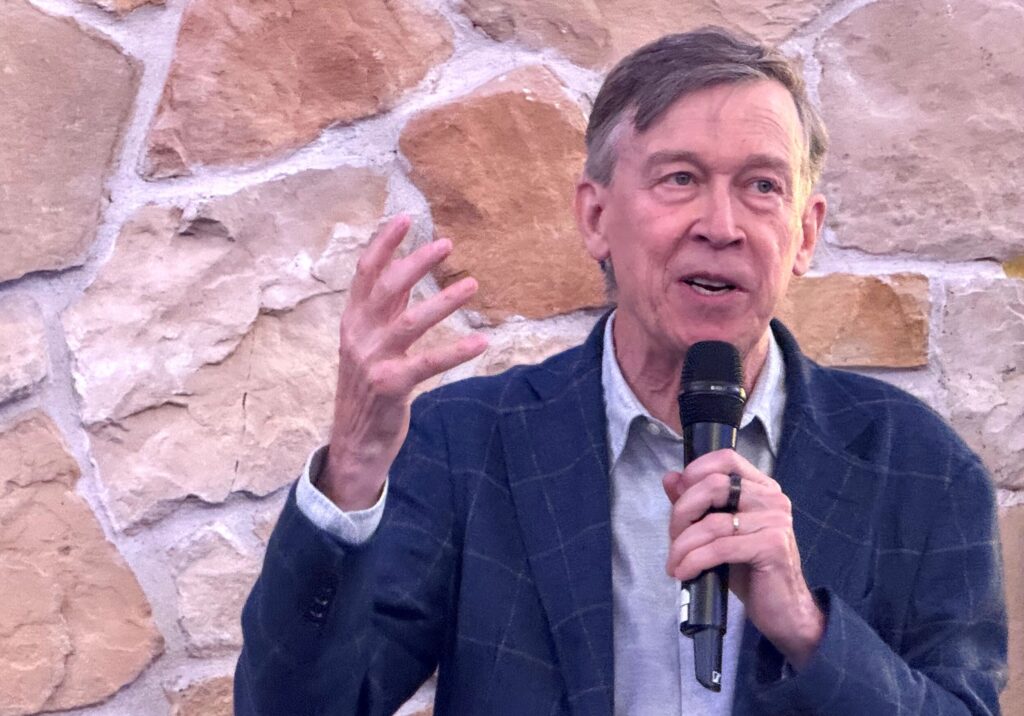
Christian Thurstone, the behavioral health chair at Denver Health, said the hospital, which is the second-largest in the state, has not seen a significant increase in therapy sessions for Medicaid patients since the 2022 law went into effect.
In fact, Thurstone said, the number of Medicaid patients who received over 24 therapy sessions for substance abuse decreased from 2020 to 2024.
“The bottom line is, we didn’t really see a big increase in patients coming for more than 24 visits when the prior authorization went away in 2022,” he said. “Maybe some other places have seen a significant increase, but that is not our experience at Denver Health.”
As a mostly publicly-funded hospital, Thurstone said Denver Health is conscientious to be “good stewards” of taxpayer money.
“We make sure we’re not doing sessions that we don’t need to, and if somebody has achieved benefits and achieved their goals, we encourage them to taper off in terms of the frequency of their sessions, so we’re pretty careful about that,” he said.
Like many other behavioral health care providers in Colorado, Denver Health has invested in community-based care to keep patients out of the hospital and lower costs, he said.
“We made a lot of investments in things like case management, peer support, and getting people engaged in recovery services, and I think some of those efforts may also limit the number of actual treatment encounters that we have to do,” Thurstone said.
Thurstone agreed with Bates’ worries about patients needing significant amounts of therapy sessions: “If somebody’s doing great, why would they want to even come to therapy?”
“We would encourage them to taper off and maybe see me once a month or once every other month just to check in, because we have a waiting list and we don’t want to keep people in treatment unnecessarily, we want to offer care to the people who are on our waiting list,” Thurstone said.
Therapy can be helpful for some individuals experiencing mental health or substance use issues, but Bates believes the state is severely lacking in alternative options.
“What we’ve seen, unfortunately, is that when we’ve tried to just say, ‘Okay, we want a lot more providers and a lot more services’, we just ended up with a lot more therapy, which is important, but it cannot be the answer to all of our community-based problems, right?” Bates said. “We have to make sure that there are recovery services, safe places to go where you don’t have to drink or do drugs to have a good time in Colorado, and I think we’ve been over-reliant on these outpatient psychotherapy services.”

Just not enough
While larger providers like Denver Health don’t expect to see significant changes with the implementation of prior authorization requirements, some smaller organizations are worried about how it could impact operations and the quality of patient care.
Corinthiah Brown, who serves as the executive director of The Don’t Look Back Center, an Aurora-based nonprofit that provides mental health and substance use treatment for women and transgender individuals, said she is frustrated to hear about upcoming changes, especially because nearly all of her clients are on Medicaid.
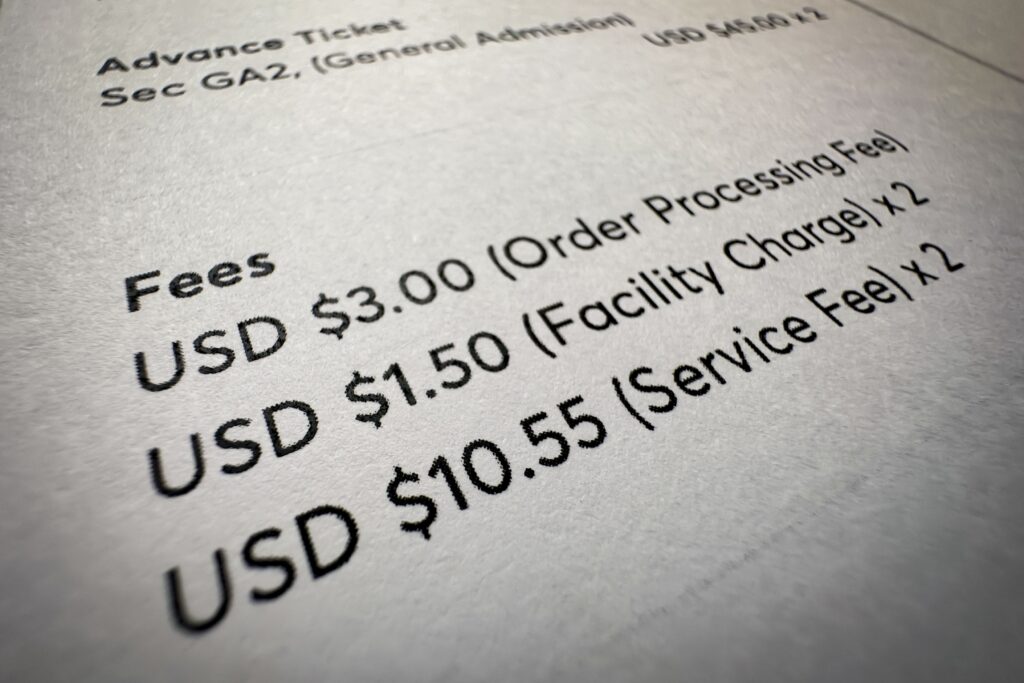
“Twenty-four sessions is just not enough for someone,” she said. “How are we gonna be able to bill for these necessary services and have someone in these programs in the different levels of outpatient if they can only have 24 sessions in a year?”
Many of the nonprofits’ clients are dealing with co-occurring issues like addiction, involvement in the criminal justice system, and mental health conditions, she said. These are often treated separately, meaning the group frequently bills Medicaid for well over 24 sessions a year for an individual patient.
Once the prior authorization requirement goes into effect, Brown said she’s worried that some of her clients may be forced to choose between treatments to stay within the session limits.
Even if patients choose to receive more than 24 sessions, Brown is also worried about them having to take a break from therapy while they wait to receive prior authorization, which can take up to two weeks.
“It puts people on hold and interrupts the therapeutic process,” she said.
More prior authorization requests means more hours Brown will have to pay her biller for, creating more costs.
“It’s not that we don’t want her to get paid, but it just puts stress on our organization because we’re a nonprofit and we have limited funding,” Brown said.
Brown said she didn’t feel like the Department of Health Care Policy and Financing listened to smaller providers when deciding what changes to implement. It is too late to do anything at this point, she said.
“We’re prepared to accept that this is what they’re going to do and we really don’t have a say,” she said. “It sounds like they’ve already made a decision.”